IV/Home Infusion Therapy Services
At Home Health Solutions Group we offer IV / Home Infusion Therapy for clients of all ages.
Sometimes when people become very ill with a complex disease, they cannot eat, let alone take medications orally.
In addition, some medications cannot be given orally because the stomach acids will destroy them, and they will no longer
be effective to treat your disease. There are many reasons why medications are introduced into the body other than through
the mouth.
What is Infusion Therapy?
Sometimes when people become very ill with a complex disease, they cannot eat, let alone take medications orally.
In addition, some medications cannot be given orally because the stomach acids will destroy them, and they will no longer
be effective to treat your disease. There are many reasons why medications are introduced into the body other than through
the mouth.
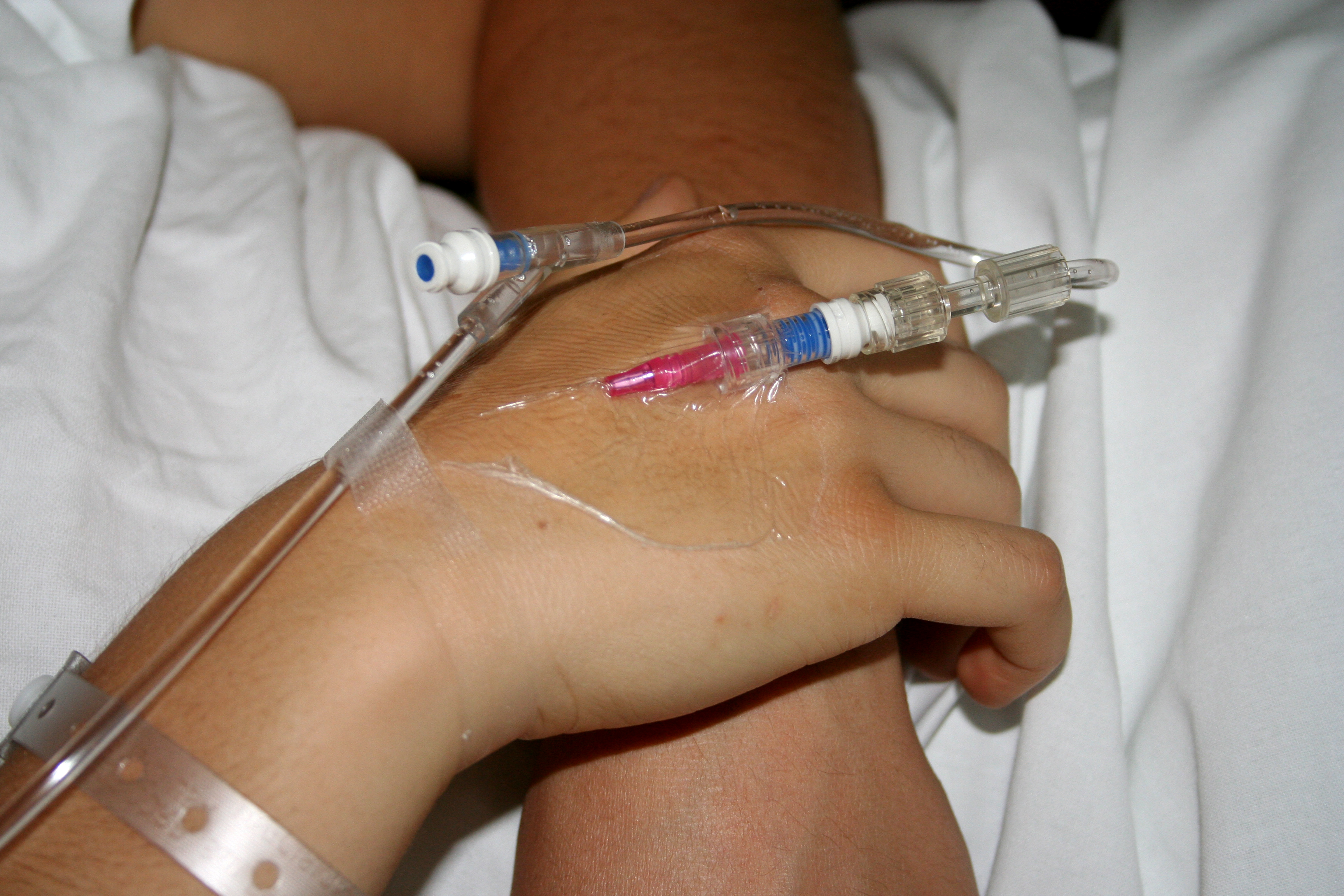
An alternative to oral treatment is infusion therapy, administering medication through the use of a sterile catheter
that is inserted into a vein and secured. This treatment method has traditionally been used only in hospitals, but now infusion
therapy can be administered in outpatient infusion therapy centers, or even in your home by specially trained nurses. These
nurses have been licensed by the state board of pharmacies, meeting the strict standards and regulations set by the board and
by the government.
What Does Infusion Therapy Treat?
Infusion Therapy is usually employed to treat serious or chronic infections that do not respond to oral antibiotics.
Cancers and the pain caused by cancers; diseases of the gastrointestinal tract; dehydration caused by nausea, vomiting and
diarrhea; and other serious diseases, such as Crohn's disease, are typical examples. Additional complex illnesses that respond
best to intravenous medications include: multiple sclerosis, some forms of arthritis, congestive heart failure and some types
of immune deficiency disorders. Certain congenital diseases require intravenous medications as well.
Some examples of infusion therapy include:
- Antibiotic/Antiviral
- Anti-Coagulation Therapy
- Anti-Emetics
- Anti-Fungal Therapy
- Anti-Hemophilic Factors
- Blood Component Stimulating Factor
- Chemotherapy
- Enteral Nutrition
- Hydration
- Inotropic Therapy
- Maintenance of Central Lines
- Pain Management
- Total Parental Nutrition (TPN)
Our highly skilled intravenous nurse clinicians are available 24 hours a day, 7 days a week. Our nurses are both IV and
chemotherapy certified and are proficient in all aspects of home intravenous therapy. The nurses coordinate your care at home
with your physician and will monitor laboratory values in conjunction with our pharmacy staff to ensure the maximum quality of
care is achieved.

Pain Management Care Services
Pain management is a significant therapy in the home infusion market. The number of clients treated at home with severe pain
requiring parenteral pain medications has increased over the past decade.
Pain is nearly a universal phenomenon and is a primary reason for seeking healthcare.
About one-third of all Americans will experience severe pain at some point in their lives.
Each year, about 25 million Americans experience acute pain and 50 million suffer from chronic pain.
In 1992, the Agency for Health Care Policy and Research (AHCPR) developed a clinical practice guideline for pain management
after several studies reported inadequate postoperative pain control. The treatment of pain has become a focus of many
accreditation organizations. Pain Management is so important that it has become one of the client’s rights that must be
discussed with clients upon admission to a home care organization for any service.
In part, the renewed focus on pain management resulted from rather abysmal accounts of adequate pain relief. In a 1999 survey,
only one in four individuals who were experiencing pain received appropriate therapy.
In part, the renewed focus on pain management resulted from rather abysmal accounts of adequate pain relief. In a 1999 survey,
only one in four individuals who were experiencing pain received appropriate therapy.
The philosophy underlying pain management has changed dramatically over the past two decades. Out of concern over the perceived
addictive properties of pain medications, before the 1990s, pain medications were largely given “as needed,” pharmacological
properties of the drugs were not given adequate consideration and limited drugs given on rigid schedules were considered the
normal course of therapy.
The new emphasis on pain assessment is best summed up with the slogan: “Pain is the fifth vital sign.”
What is pain?
Today, pain is recognized as a subjective experience that requires an individualized approach to treatment. Perhaps the most
well known definition of pain is Margo McCaffery’s: “Pain is whatever the experiencing person says it is, existing whenever he or
she says it does.” The International Association for the Study of
Pain (IASP) defines pain as “An unpleasant sensory and emotional experience associated with actual or potential tissue damage,
or described in terms of such damage.” Regardless of which definition is used, the perception of pain and its severity is a
subjective experience. Healthcare personnel may observe signs and symptoms that indicate pain or discomfort such as grimacing,
restlessness, diaphoresis and moaning, but the severity can only be reported by the client.
Pain Mechanisms, Pathways, and Nociception
The medical term for pain is nociception. Nociception is defined as the detection of tissue damage or injury by peripheral
nerve fibers.
Nociceptors are sensory receptors that detect chemical, thermal or mechanical damage to tissues. Generally, pain is described
in terms of four processes:
• Transduction • Transmission • Perception • Modulation
Transduction is conversion of the energy from a chemical, thermal
or mechanical damage to tissues into electrical energy by sensory receptors called nociceptors.
Upon activation, signals from the nociceptors travel along two major types of fibers: slow conducting, unmyelinated C-fibers,
and rapid conducting myelinated A-delta fibers. When injury occurs at the tissue level, inflammatory mediators, such as
prostaglandins, bradykinin, histamine, serotonin and cytokines are released. These substances can also trigger nociceptors.
Transmission occurs when nerve impulses from the periphery are transmitted to the spinal cord and brain. The majority of nerve
impulses travel from the periphery via the axons of primary afferent neurons and arrive at the dorsal horn of the spinal cord. From
there, nociceptive impulses travel to the thalamus and other areas of the brain.
Perception occurs when the person becomes aware of the unpleasant sensation or negative emotion and perceives it as a threat.
This sensation or perception involves both cortical and limbic structure. The perception of pain
can be mediated by the social and environmental context in which it occurs and is very individualized.
Modulation of pain occurs at peripheral, spinal and brain levels. Perhaps best known is Melzack and Wall’s Gate Control Theory
which viewed pain modulation as descending inhibitory input. Current models of pain modulation now include both inhibitory and
facilitory pathways.
Knowledge of the mechanism of pain is important in treatment because pain medications can target pain at each of the stages
of nociception. The table below illustrates the types of pain medications or therapy approach that might be selected to target
specific stages of pain:
1. Superficial Somatic — arises from skin, mucous membranes and subcutaneous tissue
2. Deep Somatic — arises from muscles, tendons, joints and bones
3. Visceral — arises from visceral organs
Management of Clients with Pain in the Home Setting
Clients identified for parenteral pain management at home must be thoroughly assessed to determine their current level of acuity
to ensure they are proper candidates for a home care referral. The following factors must be considered to determine the
appropriateness and safety of care at home:
- Conventional therapies with oral, transdermal, I.M. and rectal medication have been utilized at the highest dose without relief
of pain.
- Conventional therapies are not a reasonable choice based on patient-specific conditions, i.e., chronic emesis, loss of
absorptive bowel surface, etc.
- A client has a reliable caregiver/ family member who understands the potential problems associated with parenteral opioid
therapy.
- The client/caregiver is willing to maintain the vascular access device and pump as instructed by a nurse.
- The client/caregiver or immediate family members are not at risk for drug abuse/ misuse.
- The physician treating the client will work reliably with the home care staff and will: respond to monitoring
problems and/or ongoing assessments, and fullfill requirements for narcotic prescriptions.
- Respond to monitoring problems and/or ongoing assessments.
- Fulfill legal requirements for narcotic prescriptions.
- The home setting is appropriate and safe for administration of pain management therapy.
Nursing Considerations

The home care nurse is a valuable resource for the family and physician to ensure that
pain management therapy is effectively and safely administered. Nurses use a holistic
approach to the client who is receiving home parenteral pain management including the physical, emotional,
social and psychological aspects of this therapy.
Pain assessment is an integral part of a generalized body system assessment that occurs during each
home visit. Pain assessment typically involves a number of areas that include:
-Pain characteristics — the onset, duration, location, quality, intensity, associated symptoms and factors that help to
alleviate or exacerbate pain.
- Management strategies — a history of how the patient has managed pain including all medications (prescribed and over-the-
counter), non- pharmacological treatments, coping strategies and family and/or community support utilization.
- Relevant medical history — any illnesses, medical diagnoses, injuries, surgical procedures, psychiatric illnesses or
accidents.
- Relevant family history — general health and availability of family members, family history of pain and pain management.
- Psychosocial history — marital or vocational problems, stressors or depression.
- Impact of pain on the client’s life — impact on work, daily activities, personal relationships, sleep and appetite.
- Client’s expectations and goals — goals for pain management and acceptable level of
pain intensity, effect of pain management on ADLs, social and emotional well-being.
During pain management therapy in the home, nurses routinely assess the level of the client’s pain. A variety of tools
are available to assess pain; these include numerical rating scales (0 to 10), visual analog scales (asking the patient to rate
the level of pain along a 10 cm line), categorical scales (such as the Wong-Baker faces) and multidimensional
tools such as the McGill Pain Questionnaire or the Brief Pain Inventory. Most important is that these tools are consistently.
used so that an accurate assessment of pain management effectiveness over time can be determined.
In addition to assessment of the patient’s pain, the home care nurse also teaches the patient how to use the infusion pump or
administer the parenteral pain medication, how to care for the vascular access device, signs and symptoms to report to the
nurse and physician, and how to safely store the equipment and supplies associated with this therapy. The nurse also assesses
the effectiveness of the plan of care and the effect of the therapy upon the family or household.
At Home Health Solutions Group, we specialize on Pain Management Care for patient at home.
Call Today 786-991-2300
Personal Service
Patient Care Liaison personnel are willing to meet with clients or their representatives in the comfort of their homes or institution.
